In the first two months of 2019, Canada has seen an increase in the number of active measles cases compared to the same period last year. There are currently ten confirmed cases in British Columbia, enough for the Provincial Health Services Authority to declare an outbreak, and one in Quebec and Ontario, each. For a country like Canada, which declared itself free of measles in 1998, the slow, but steady increase in the number of measles cases per year is a disturbing trend.
The highly infectious and contagious illness is contracted when a person makes contact with the measles virus. Spread via the respiratory tract, the measles virus can remain infectious in the air for up to two hours, making the possibility of contraction very high in densely-populated regions. Measles, like other respiratory viruses, presents a standard set of symptoms including a high fever in excess of 40 degrees celsius and a dry cough, but is punctuated by a characteristic skin rash covering a large area of the body.
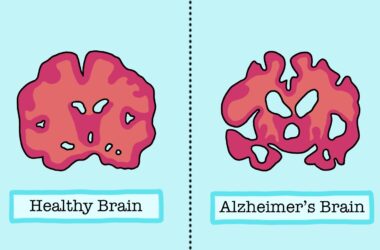
“It is probably one of, if not the, most infectious virus[es] known,” Brian Ward, an associate professor at the Centre for the Study of Host Resistance, said. “Before HIV, [measles] was considered to be the most immunocompromising virus around.”
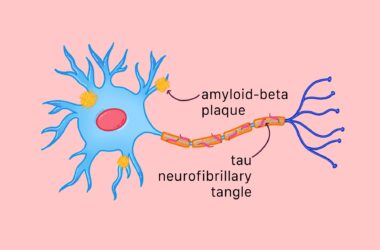
Measles replicates in host cells via a single-stranded ribonucleic acid (RNA) pathway, a method of replication in which the virus harnesses multiple sets of proteins to survive. According to the modern classification system of viruses, this places measles in the same viral replication category as rubella and the mumps viruses, all of which spread quickly from host to host.
Virologists quantify the infectiousness of a disease based on its reproduction number (R number), which is the average number of people that every person with the disease will secondarily infect. The reproduction number for seasonal influenza, the common flu, is two. By contrast, the reproduction number for measles is 18.
Since the disease has scarcely appeared in Canada over the last two decades, public health workers have scrambled to identify and isolate cases of measles over the last week. Most recently, Vancouver reported ten related cases of measles thought to have been transferred through the public school system.
According to the federal government, the best defence against measles is vaccination, which is covered free-of-charge by provincial health care. For a disease with such a high R number, greater immunization coverage is required to achieve herd immunity.
“A highly-vaccinated population, where over 85 per cent, and, ideally, greater than 95 per cent of the population is vaccinated, can truncate [the] spread [of measles] dramatically,” Ward said. “Any imported case will only spread to a small number of secondary cases. As vaccine coverage drops, the outbreaks caused by each imported case become larger.”
A 2018 study in the PLOS Medicine journal confirmed reports of dropping vaccination rates across the United States.
“Since 2009, the number of philosophical-belief vaccine nonmedical exemptions (NMEs) has risen in 12 of the 18 states that currently allow this policy,” the study reads.
Commonly referred to as the ‘anti-vaxxer’ movement, many American cities are currently witnessing the repercussions of parents exempting their children from medically-advised vaccinations. Even though medical science has conclusively proven that vaccinations are overwhelmingly safe, the rate of children who are receiving optional vaccinations continues to decrease.
The Seattle, Washington region, one of the many ‘metropolitan hotspots’ for unvaccinated populations as outlined by the 2018 study, has become the epicentre of the current measles outbreak in the United States. In Washington, the majority of measles cases identified have occurred in individuals under the age of ten who had never received the vaccine.
In order for Canada to avoid falling victim to large gaps in the immunization record and to protect at-risk populations such as the immunocompromised and elderly, children need to remain up to date with all types of vaccinations.
“The worst outcome of measles in Canada would be [the] hospitalization of patients with pneumonia or [another] secondary bacterial infection,” Ward said.
The fateful consequences of having an unvaccinated population would have the greatest negative effects on those Canadians most vulnerable in the first place.