A cancer diagnosis can radically change the course of a person’s life. Nearly one in two Canadians is expected to develop cancer over their lifetime, and one in four is expected to die from it. Fortunately, physicians have an increasingly effective array of treatments available to counter this devastating disease.
Three types of receptors are commonly found on the surface of breast cancer tumour cells: Estrogen, progesterone, and HER2 protein receptors. These receptors fuel the growth of cancer cells. Existing therapies can block any of these receptors and successfully stop the growth of the tumour. However, none of these receptors are present in one specific subtype of breast cancer called triple-negative breast cancer (TNBC). It is the most aggressive subtype of breast cancer and it accounts for about 15 per cent of all cases.
The problem with TNBC is that cancer cell growth is not due to any of the three receptors, so current targeted therapies that block the typical receptors are not effective. The way these tumour cells grow is not yet well understood.
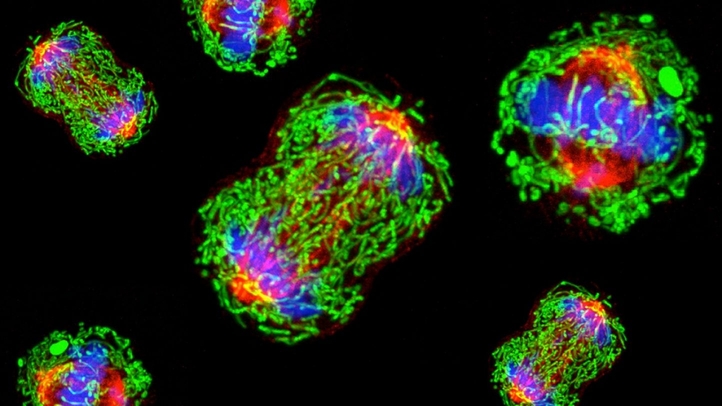
Recently, a team of researchers led by Dr. Jean-Jacques Lebrun, a senior scientist in the Cancer Research Program at the Research Institute of the McGill University Health Centre (RI-MUHC) and a professor of medicine at McGill University, discovered novel mechanisms through which TNBC tumour cells grow. The team used a state-of-the-art gene-editing technology called CRISPR to screen the entire human genome and successfully identified two key pathways that allow TNBC tumours to grow and propagate.
“There are absolutely no targeted therapies for this type of cancer,” Lebrun said in an interview with The McGill Tribune. “Patients will undergo chemotherapy or radiotherapy, both of which are largely inefficient.”
The two pathways they identified include an oncogenic pathway named mTOR and a tumour suppressor pathway named Hippo. Both pathways play a role in the regulation of cell growth and programmed cell death, called apoptosis. In TNBC cells, the pathways become abnormally activated, leading to uncontrolled cell growth and tumourigenesis.
The identification of these two growth mechanisms was a major step forward in the search for a TNBC treatment.
Lebrun and his team subsequently investigated possible ways to interfere with these growth pathways in a recent study published in Nature Communications. They found two potential drugs that would accomplish the necessary interference: Torin1, a drug known to block the mTOR pathway, and verteporfin, a drug normally used for retina eye diseases that can mimic the Hippo pathway.
According to Dr. Meiou Dai, a research associate in the Lebrun Lab at the RI-MUHC and first author of the study, preliminary research has shown some very encouraging results.
“Torin1 led to growth inhibition on the cell models, and verteporfin was able to induce apoptosis in cancer cells,” Dai said in an interview with the Tribune.
Their results show that these two drugs are effective at countering the growth of TNBC cancer cells. They also demonstrated that both drugs act synergistically and have an even better outcome when used as a combination therapy.
Lebrun and his team also tested the drugs for other breast cancer subtypes and found that they were all being affected by their combination therapy.
Although this study has paved the way to an effective targeted therapy for TNBC, there is still work to be done before it can become approved. Trials must be conducted on patients to examine the effectiveness of the combination therapy in humans. However, the fact that these are already known drugs is an important advantage.
“One [verteporfin] is already approved for an eye disease while the second [Torin1] is currently being tested in clinical trials,” Dai said. “This is very important because it should really shorten the time it will take for the proposed combination therapy to be approved and start benefiting patients.”