On May 31, a research team at the Montreal Heart Institute (MHI) became the first in Canada to implant a new cutting-edge biological prosthesis into a patient’s heart. The main purpose of the device is to substitute a faulty aortic valve—a valve that regulates blood flow between the heart’s main pumping chamber (left ventricle) and the main artery (aorta). After a defective aortic valve has been removed from the heart, the prosthesis acts as its replacement.
The novelty of this device is that the replacement tube and valve come pre-assembled, reducing the time patients spend on the operating table and minimizing the risk of technical errors by surgeons. However, according to Renzo Cecere, the director of cardiac surgery at the McGill University Health Centre (MUHC), the new valve generally shares the same design as older models.
“The advantage now is that we have this conduit that comes pre-packaged and pre-built with a biological valve contained within the conduit,” Cecere said in an interview with The McGill Tribune. “But conceptually, there is nothing new or brilliant about this, it just has not been available on the market.”
Still, the new device is likely to help many patients suffering from aortic valve disease: In 2017, faulty aortic valves accounted for over two-thirds of all valvular heart disease deaths in the United States.
Valvular heart disease occurs when the aortic valve does not open or close properly. The valve consists of three flaps that open and close together with each heartbeat and acts as a “gatekeeper” by controlling how much blood flows from the heart to the rest of the body. If the valve is diseased, it becomes either too narrow and stiff to fully open (stenosis) or too wide to close completely (regurgitation), causing some blood to flow backwards. Sometimes, valves can also be malformed due to a birth defect called congenital heart disease.
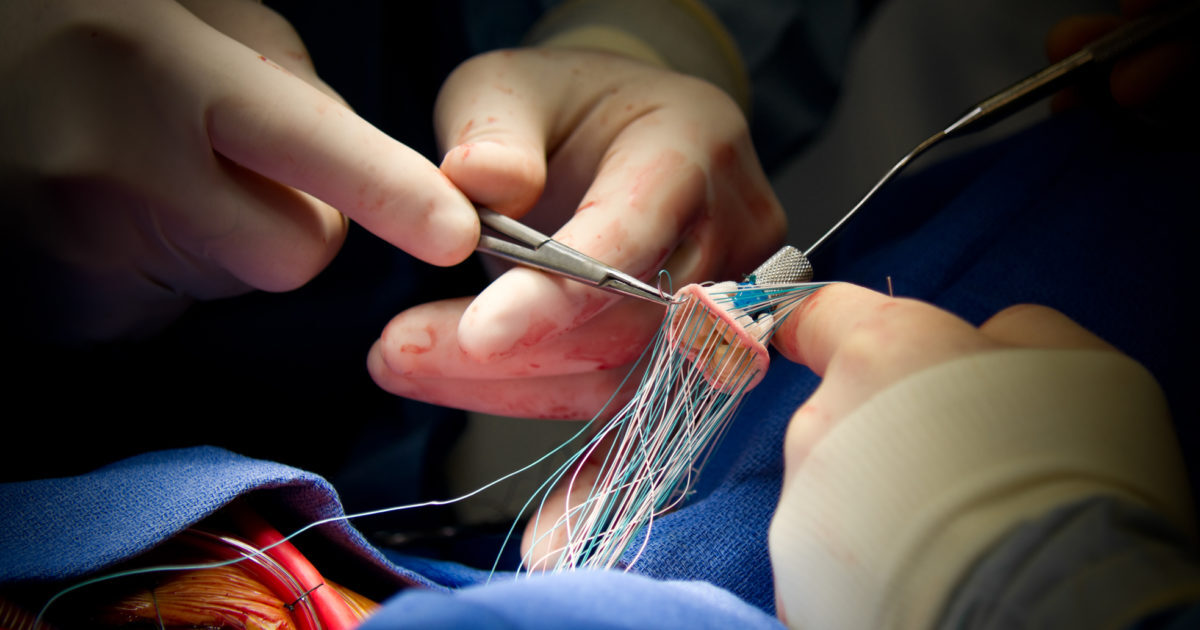
Given the prevalence of diseased aortic valves, replacing them is a common operation known as the Bentall Procedure. The process involves removing the aortic valve and root and then implanting an artificial tube with a mechanical or biological (tissue) valve inside of it.
Until recently, surgeons have had to sew the valve into the tube before inserting it into the patient’s heart. This step of the procedure is complex, time-consuming, and carries the risk of surgeons making technical errors when stitching the tube and valve together. This new prosthesis, however, eliminates this step with it being pre-assembled and therefore ready to use.
Fortunately, this device will soon be offered to patients in the MUHC: Cecere has already submitted a formal request to acquire it. However, only a select number of patients could qualify as good candidates for this device—even though the MUHC performs about a thousand heart surgeries a year.
“There are a lot of things we do that are quite niche and not high-volume activities,” Cecere said. “But nevertheless, the patients need to be served. It is our obligation to make sure we have the right tools on the shelf.”
For Cecere, this device is further evidence of the remarkable progress that medical technology has made since he became a cardiac surgeon.
“Whether it is in coronary disease, valvular disease, heart failure, or artificial heart technology, all of them have made a tremendous evolution in the last 15 to 20 years,” Cecere said. Indeed, the first aortic valve replacement was performed in 1962 and now, nearly 60 years later, there is a pre-assembled prosthesis that can be implanted into a patient’s heart in 2.5 hours.