If you have ever watched the television series Monsters Inside Me, you may be familiar with parasitic worms. Each episode features a dramatization of an infectious disease case, with an accompanying explanation of its cause. Cases dealing with parasitic worms range from a teenager infected with the parasitic worm, Trichinella spiralis, after eating uncooked meat, to a man with worms feeding in his brain. A common question that always arose in my mind was the following: “How do these worms manage to survive?”
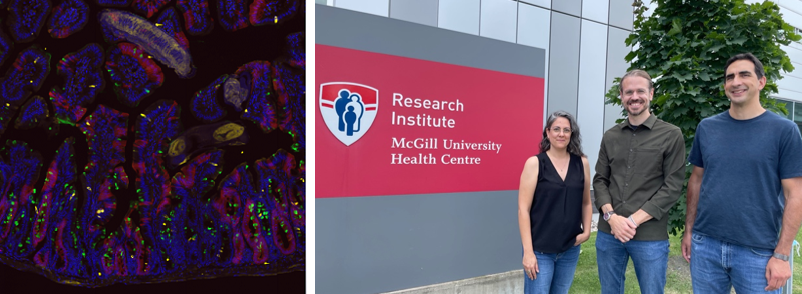
A recent study published by a group of McGill researchers in the Journal of Experimental Medicine aimed to answer that very question. Irah King, an associate professor in the Department of Microbiology and Immunology, led the study along with his lab at the Research Institute of the McGill University Health Centre (RI-MUHC).
Parasitic worms, also called parasitic helminths, are known to evade the immune system of the individuals they infect. Many of these helminths begin their attack in the gut epithelium—a layer of cells that line the intestines—before progressing to other areas. The epithelium is made up of many cells, including intestinal stem cells (ISCs). These cells are “fetal-like” in that they have the capability to develop into various cell types, compared to the other more rigid, stuck-in-their-ways, “adult-like” cells in the intestine.
The gut epithelium also has some innate defence and repair mechanisms in response to foreign invaders. The primary defence mechanism is the type 2 immune response in which goblet cells, a cell important for nutrient digestion in the intestines, produce mucus to trap the invader. This type 2 immune response is activated by cytokines, molecules that increase the body’s immune responses, such as IL-4 and IL-13. During the injury process, the epithelium may undergo severe damage, which mostly leads to a severe decrease in ISCs. The epithelium repairs itself by reprogramming the “‘adult cells” into “fetal cells” so that more cells can be generated.
But while these repair and defence mechanisms are well-studied, it is not known how they are affected during a helminth infection.
To study this, King and his team infected mice with a roundworm called Heligmosomoides polygyrus bakeri (Hpb). They removed the intestine cells from the animal models and grew them in Petri dishes until they formed organoids—three-dimensional cell cultures derived from animal or human tissues. They then looked at the gene expression within the organoids and found that the gut cells of the infected mice had more helminths than non-infected mice and expressed fetal-related genes.
Their finding shows that helminths trigger the repair process in the intestine by activating fetal genes. However, researchers also found that helminths suppressed the type 2 immune response. Mice that were genetically engineered to have lowered type 2 response had increased fetal gene expression in their organoids after Hpb infection. Those with a normal type 2 response did not show any fetal gene expression.
The results reveal two interesting ways those pesky helminths manage to evade immune responses: The worms first evade immune response by decreasing type 2 immunity in the body of their host. They also reprogram the intestine, so it goes into a repair state, while allowing the helminths to persist within the intestine.
“This study establishes the fact that helminths are able to directly regulate their host epithelium. Since the epithelium is at the forefront of host-parasite interactions, this suggests that manipulating these interactions can result in the discovery of new anthelmintic drugs,” Danielle Karo-Atar, a postdoctoral fellow at the King lab and first author of the study, wrote in an email to The McGill Tribune.
However, Karo-Atar notes that more progress is needed before these new pathways can inform any kind of treatment.
“Future directions for this study will be to identify the molecular mechanisms responsible for this worm-induced fetal-like reversion of the epithelium,” Karo-Atar wrote. “In addition, we would like to understand if and how worms are enhancing intestinal resilience and identify the pathways responsible.”