On March 26, 2024, the Annual George Karpati Lecture invited Dr. Rita Horvath from Cambridge University to speak on mitochondrial medicine—to share her expertise on everything from mechanisms to treatments. Horvath has spent over 25 years studying genomics and biochemistry for the diagnosis and treatment of rare neurological disorders.
The lecture series focuses on recent developments in neuromuscular disease research and treatment, honouring George Karpati, who was a well-respected clinical neurologist at The McGill Neuro. Horvath commenced her presentation by reminiscing about her first encounter with George Karpati in Montreal, which happens to have been almost exactly 30 years ago.
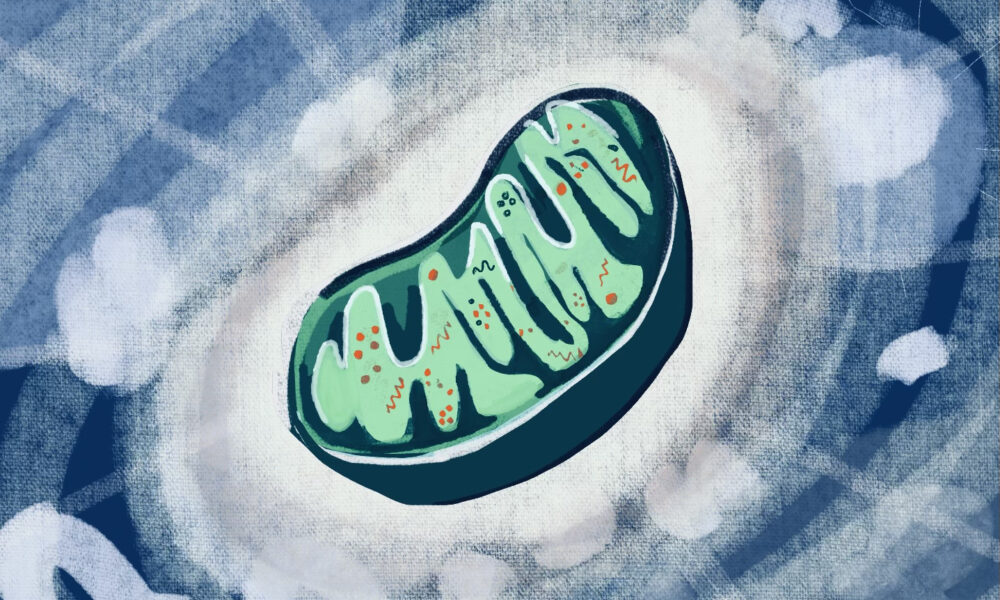
The mitochondria, often referred to as the “powerhouse of the cell,” perform a large array of crucial cellular functions such as calcium ion storage for cell signaling activities and regulation of cell growth and death. Mitochondrial medicine is an umbrella term for mitochondrial diseases, including mitochondrial disorders and syndromes, along with their biochemical treatments.
The deletions or low amounts of mitochondrial DNA (mtDNA) have a variety of causes, such as simply a low production of mtDNA, or other rare genes. The deletion mechanisms of mtDNA in mitochondrial diseases have been studied, including mitochondrial nucleotide salvage pathways, to better understand the causes. Dr. Stefanie Bulst, a Medical Centre of Genetics researcher, discovered alongside her research group that the supplementation of deoxyguanosine phosphate and deoxyadenosine phosphate (dAMP/dGMP)—DNA’s building blocks—leads to partial rescue of mtDNA copy numbers, to make up for its low supply, a potential treatment to mitochondrial depletion syndromes.
Alpers’ syndrome is an example of a genetic neurodevelopmental disorder that Hovarth works with, caused by the depletion of mtDNA and which may appear without any genetic history. More specifically, the syndrome occurs as a result of mutations in the polymerase gamma gene (POLG), which encodes mitochondrial DNA polymerase. It typically manifests between the ages two and four, or between ages 17 and 24, causing symptoms like seizures and stunted growth.
Surprisingly, “not only the deletions or lacking of genes but also an excess of mitochondrial DNA can lead to issues, or develop symptoms,” Horvath mentioned in her lecture.
Mitochondrial neurogastrointestinal encephalomyopathy, MNGIE in short, illustrates an example of diseases that arise from an excessive number of genes. As the name of the disease suggests, it is characterized by symptoms spanning the degeneration of muscles, affecting a variety of physiological systems, from the patient’s digestive tract to eye movements. The disease is progressively degenerative and has an average life expectancy of 37.6 years.
Treatment approaches for mitochondrial diseases as well as the diseases themselves vary widely. Current research findings suggest that bacterial endonucleases, which are bacterial enzymes, can be used for mtDNA gene editing, meaning that they can cleave mutant mtDNAs.
“They can robustly eliminate mutant mtDNA allowing the wild type [the normal form of the gene] to repopulate the cell. Using cytosine base editors, you can also edit mtDNA to correct mutations,” Horvath said.
Another effective treatment is through using cytosine base editors, which has enabled correcting the mtDNA mutations. Moreover, next-generation sequencing has been found to aid the diagnosis of mitochondrial diseases, with whole-genome sequencing offering insights into individual mitochondrial diseases.
An experiment conducted at Horvath’s lab, led by research associate Denisa Hathazi, grows brain organoids—a lab-grown 3D tissue resembling human brain—with patient stem cells to study disease characteristics.
“Though limited to 200 days of growth [and] thus not fully representing deep brain neurons, these organoids are still a valuable model for investigating various neuronal cell types together,” Horvath explained.
Because of the rarity of mitochondrial diseases, there are challenges in research such as recruiting participants for clinical trials for treatment developments. However, some significant progress has been made in the past decade. Specialized clinics such as the LifeArc Centre in the UK are emerging to continue research on diagnosis and identification of disease progress for mitochondrial diseases. Horvath’s aspiration to establish a clinical database for rare neurodegenerative diseases emphasizes the unwavering efforts to improve patient outcomes.