Sixty-five years and four Nobel Prize nominations after Dr. Thomas Chang invented the first artificial cell in his McGill dorm room, the invention is still improving lives in countless new ways. From blood transfusions to cancer suppression and, most recently, COVID-19 treatments, Chang’s invention continues to push the boundaries of medical possibility.
Chang developed the first crude prototype of an artificial red blood cell during his undergraduate studies at McGill.
“It was back in 1957 and I worked […] in my dormitory room in Douglas Hall,” Chang said in an interview with The McGill Tribune. “I [did] my research in my bedroom and when people [were] not there, I used the living room.”
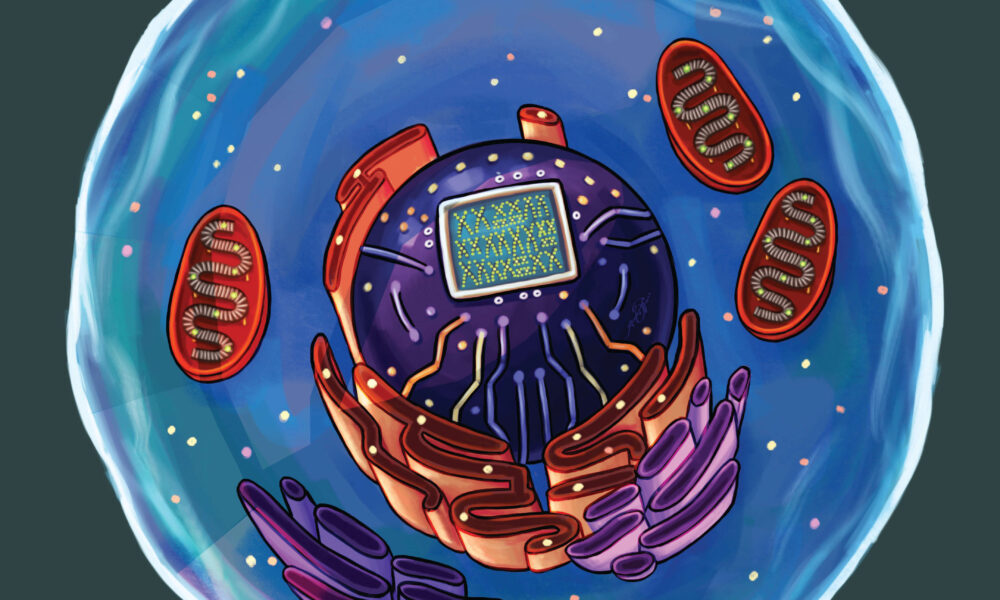
Chang’s artificial cells are not just physical entities. They are artificial and modifiable structures that can replace or supplement malfunctioning cells. The cells consist of an artificial membrane made of several types of polymers,, and/or crosslinked proteins that surround typical cell components like enzymes, proteins, other cells, and more. Artificial cells act as mini bioreactors—or reaction chambers—where molecules can enter and react with the contents inside before being exported once again.
Artificial cells are uniquely useful because their membranes and contents can be modified to suit many needs.
“We can prepare them to contain cells, stem cells, vaccines, mRNA, DNA, microorganisms, magnetic material, absorbents, hormones, drugs, and other material,” Chang said. “There are unlimited possibilities in variations for the artificial cell membranes and contents.”
According to Chang, artificial cells that contain hemoglobin and other proteins mimic blood cells but do not belong to any blood type group, making them a universal blood substitute. This is especially useful for emergency trauma cases when on-site blood cross-matching is not available, and for people who cannot accept blood transfusions for religious reasons. And since the membranes do not have antigens—which can sometimes cause the body to reject foreign substances—the artificial cells will not be attacked by antibodies or white blood cells. Beyond their use as a blood substitute, this makes them ideal to carry essential enzymes or substances into the body without the risk of adverse effects.
“As a physician-researcher with the aim to do what is best for the patients, my plan has been to continue to do frontier innovative research […] and at the same time to encourage others around the world to develop these ideas for patient use,” Chang wrote in a statement to the Tribune.
According to Chang, artificial cells have already been used as a delivery vehicle for mRNA vaccines. They have also been used to treat patients with COVID-19. These patients can develop a cytokine storm—a fatal release of excessive cytokines due to an overreaction of the immune system. Cytokines, small proteins that control the growth of blood and immune system cells, are more effectively removed by activated charcoal than traditional hemodialysis. Activated charcoal, however, can release harmful particles into the body and damage red blood cells. By using an artificial ultrathin membrane to coat the charcoal, those negative side effects can be avoided while also increasing the speed at which cytokines are removed from the blood.
“A problem is a challenge, and challenges mean that you can innovate.”
– Dr thomas Chang
In a 2021 paper, Chang’s artificial cells showed promise in suppressing skin cancer. Inspired by a 2005 study that found that low levels of the amino acid tyrosine suppress melanoma tumor growth, Chang began working on a nanobiotherapeutic PolyHb-tyrosinase, an enzyme that lowers levels of tyrosine in systemic circulation to inhibit tumour growth in mice. Overall, their results showed that nanocarrier PolyHb-tyrosinase suppressed tumour growth in mice and even inhibited tumor cell migration, also known as metastasis.
“We have only touched the surface of the potential of the extension, innovations and uses of artificial cells,” Chang wrote. For Chang and others working on the cutting edge of biomedicine, there is much more to learn.