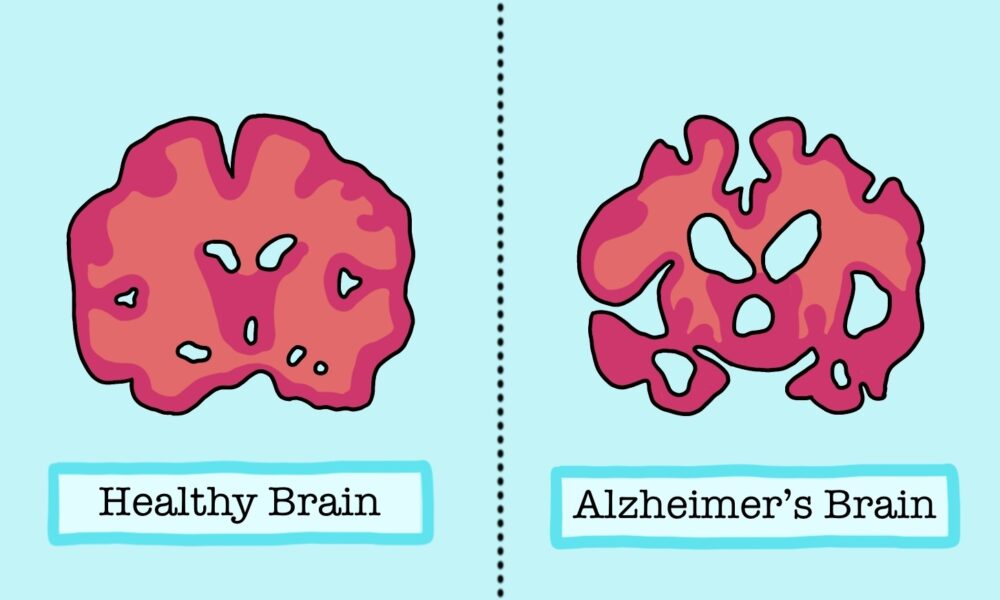
Healthcare inequities—avoidable differences in health across population subgroups—are ubiquitous in Canada. Even though women are more affected by dementia—a group of age-related diseases characterized by memory decline—than men, current dementia policies often do not consider sex-based differences.
Dementia is a major public health issue, with the number of cases projected to rise significantly as the population ages. According to the Alzheimer Society of Canada, nearly 600,000 Canadians are currently living with dementia; this figure is expected to double by 2030. Women account for approximately two-thirds of all dementia cases, but an alarmingly low amount of research and policy development in the field takes gender-based disparities into account.
In a recent study, Geneviève Arsenault-Lapierre, a researcher at the Centre for Research and Expertise in Social Gerontology and an associate professor in the Department of Family Medicine, and her collaborators investigated disparities in healthcare utilization between men and women with dementia.
Expanding on previous research conducted in Ontario, Lapierre’s study examined 23 healthcare indicators such as visits to family physicians, antidepressant prescriptions, and mortality.
Pulling data from the Quebec Integrated Chronic Disease Surveillance System, Arsenault-Lapierre and her collaborators organized the healthcare indicators into five different healthcare settings that reflect a continuum of care needs: Ambulatory care (outpatient services), pharmacological care, acute hospital care, long-term care (including nursing homes), and mortality.
Their findings revealed significant differences in how men and women access and use healthcare, but the nature of these differences varied by setting.
“Women received more ambulatory care, saw their family doctor more often, and received their dementia diagnosis from their family doctor,” Arsenault-Lapierre said in an interview with The Tribune.
Moreover, women were more frequently prescribed dementia-related drugs, such as memantine and cholinesterase inhibitors. However, they also saw increased prescriptions for antidepressants and benzodiazepines—drugs that are not optimized for dementia treatment.
On the other hand, men with dementia were hospitalized more often and relied more heavily on acute care services—many of which could have been avoided with better primary care. They also experienced higher rates of hospital readmission within 30 days, an indicator of lower-quality healthcare and poorer patient outcomes.
“Men went to the hospital more often,” Arsenault-Lapierre added. “They also had more acute care services […] that could potentially have been avoided, and more [30-day] readmissions after hospitalization.”
Additionally, men with dementia were more frequently admitted to long-term care facilities and had higher mortality rates than women with dementia.
While this study was primarily descriptive and did not investigate the causes of these sex-based differences, Arsenault-Lapierre emphasized the importance of understanding how sex is recorded in healthcare databases.
“Administrative databases [use] sex attributed at birth, which changes if the person requests a change,” Arsenault-Lapierre explained. “We measure indicators that are influenced by biological factors, that is, sex, but also psychological and sociocultural factors, that is, gender.”
Nevertheless, their findings highlighted the need for healthcare policies that consider sex differences in dementia care. In particular, they support the implementation of personalized medicine—an approach that tailors treatment to the needs of individual patients rather than employing a one-size-fits-all strategy.
Personalized medicine could help address key disparities within dementia treatment practices, such as the overprescription of potentially ineffective drugs to women and the lack of adequate outpatient care for men.
To better understand how people with dementia access and use healthcare services, Arsenault-Lapierre says future work should focus on differences between additional population subgroups.
“[We should investigate] the differences at the socioeconomic level and between rural and urban areas because rural areas do not have the same services as urban areas,” Arsenault-Lapierre said.
Ultimately, further research is required to determine whether these sex differences arise from inequities in healthcare access and, if so, how to address them.