A recent study led by Filip Morys, a Research Associate at The Neuro in Montreal under the supervision of Dr. Alain Dagher, explores the bidirectional relationship between obesity and brain function. The findings reveal that weight gain can be both a cause and a consequence of changes in the brain.
“We have this bi-directional model of obesity and brain interactions where changes in the brain can be vulnerability factors for weight gain in younger adults, and in older adults, chronic obesity is actually leading to brain damage,” Morys explained in an interview with The Tribune.
In other words, brain structure and function can shape a person’s susceptibility to obesity, while long-term obesity may, in turn, contribute to cognitive decline and other neurological impairments. One key factor in this complex relationship is inflammation.
“Being obese essentially means that your body is in a constant state of low-grade inflammation because fat tissue produces substances that cause inflammation in the body,” Morys said.
While this chronic inflammatory state is known to contribute to insulin resistance and cardiovascular disease, it also appears to impact brain health.
The study found that inflammation-related changes in brain structure and function may influence eating behaviour and self-regulation, potentially creating a feedback loop that makes weight management more difficult.
To investigate these brain-body interactions, Morys’ team used non-invasive imaging techniques, including diffusion-weighted imaging, which measures water movement in brain tissue.
This allowed them to examine differences in brain structure and function among individuals with varying body mass indices (BMI), providing insights into microstructural changes linked to obesity.
“What we’re looking at is not necessarily direct inflammation,” Morys clarified. “We’re doing non-invasive brain imaging, which makes it difficult to definitively say the changes are neuroinflammation.”
Despite this limitation, their findings suggest that obesity-related brain changes may be linked to inflammatory processes, which can alter cognitive function and decision-making related to food intake.
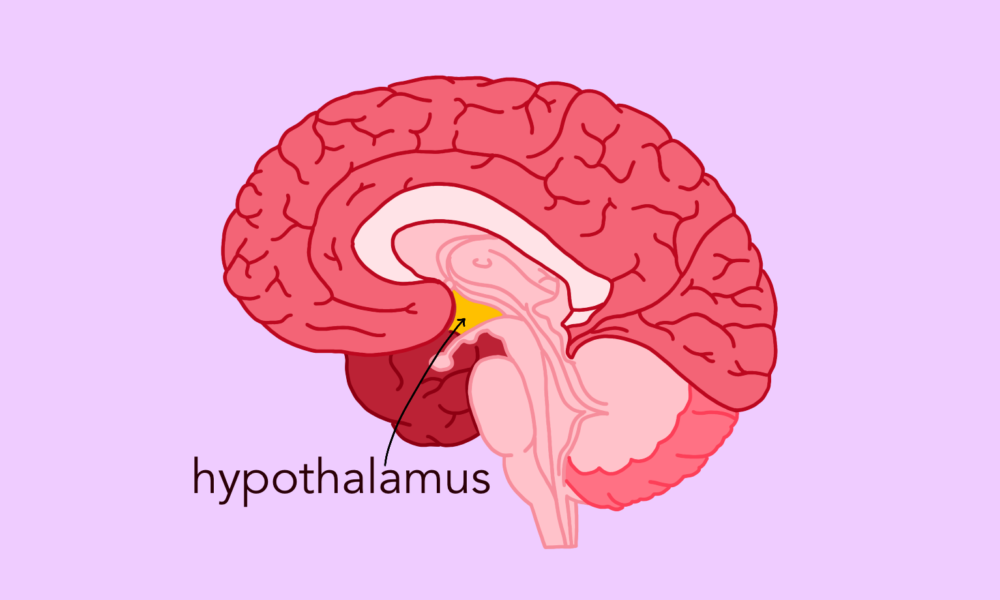
Individuals with higher BMI also tended to exhibit changes in the brain regions involved in impulse control and reward processing, areas that are critical for regulating eating behaviour. Disruptions in these networks may explain why some people struggle with overeating despite knowing the associated health risks.
Moreover, decreased connectivity between key brain areas could impair a person’s capacity to manage cravings and choose healthier foods. These findings underscore the complexity of obesity and highlight the importance of addressing cognitive and emotional factors alongside conventional weight management approaches in treatment plans.
For many years, the neurological consequences of obesity were poorly understood; however, research efforts are ramping up. Strategies like cognitive training or anti-inflammatory treatments targeting brain function may help mitigate obesity risk. In older adults, reversing or mitigating brain damage caused by long-term obesity may help slow cognitive decline and improve quality of life.
Looking ahead, Morys hopes to conduct long-term studies to track how brain function and obesity interact over time.
“Ideally, we would love to observe these changes over the course of time, starting with children and following them throughout their entire lifetime to trace how brain changes relate to body mass index and obesity,” Morys said.
Such research could yield critical insights into the lifelong relationship between brain health and body weight, paving the way for more personalized and effective treatments.
Ultimately, this study supports the idea that obesity is not simply a result of willpower or lifestyle choices, but a multifaceted condition encompassing biological, neurological, and environmental influences. By understanding how the brain influences appetite, behaviour, and metabolism, scientists can develop more holistic interventions that address the root causes of obesity, rather than focusing on its symptoms alone.