Although once upheld as an exemplary source of pain relief, opioid painkillers have quickly come to cause a deadly health emergency across North America. While in 2016 there were 2,458 reported opioid-related deaths in Canada, 2017 saw a considerable increase to 3,987 deaths. In light of this growing crisis, the Montreal non-profit Science & Policy Exchange, an organization dedicated to applying research to government policies, held a seminar on Aug. 29 with four experts sharing their perspective on the opioid epidemic.
“Canada […] has one of the highest rates of opioid-related death in the world,” Rebecca Jesseman, director and senior policy advisor at the Canadian Centre on Substance Use and Addiction, said. “The rate of deaths due to opioids is highest in British Columbia at 29 per 100,000 and in Alberta at close to 17 per 100,000. The majority of those deaths are unintentional and involve fentanyl.”
Fentanyl is one of the most frequently prescribed opioids in Canada. It is particularly infamous because of how cheap it is to illegally produce and transport. Its potency also makes even a quarter of a milligram of the drug fatal.
“Today, the illicit drug supply is becoming increasingly toxic, with fentanyl present in close to 70 per cent of opioid-related deaths reported by coroners in 2017,” Jesseman said.
Canada and the United States have some of the highest rates of painkiller prescription. Historically, they have been recommended for those temporarily suffering from severe pain, due to trauma or surgery, but there was a substantial rise in long term opioid usage after they started being prescribed to patients suffering from chronic pain. Unfortunately, research did not consider the effects of using opioids for extended periods.
“[In 2006 and 2015], authors reviewed roughly 40 randomized trials and they found that opioids are superior to placebos for pain relief […], but the problem with these randomized controlled trials is that the average duration of those trials so far has been [just] five weeks,” Marc Martel, the research director at the Alan Edwards Pain Management Unit, said. “What we’ve [now] learned is that the opioid addiction-rate in patients with chronic pain is around 10 per cent.”
Today, there is more consideration for the likelihood that an individual might become addicted to opioids, with young males and those with substance use or psychological problems being the most susceptible to drug abuse. A major factor in addiction is how the patient is weaned off of prescribed opioids.
“The abrupt discontinuation of opioid therapies can be really problematic, [and] may lead to reduced access to pain care, under-treatment of pain, and, most importantly, may lead to risky opioid-seeking behaviour,” Martel said. “Roughly 11 per cent of patients with pain who have been discontinued from opioids turn to illicit sources in order to get opioid pain relief.”
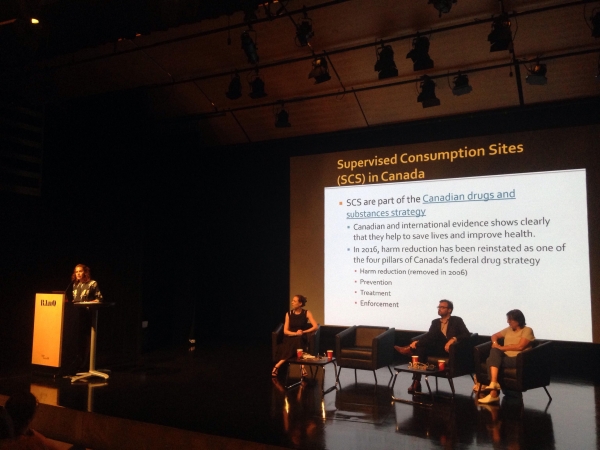
Government policy has recently acknowledged the futility of trying to prohibit addicts from further usage. In an effort to rectify the oversight, harm-reduction has become one of the four pillars of Canada’s federal drug strategy in 2016, alongside prevention, treatment, and reduction.
“The harm-reduction approach aims to assist people who use legal and illegal psychoactive drugs to live safer and healthier lives,” Sandhia Vadlamudy, executive director of Cactus Montreal, said. “In Canada, harm reduction policies include increased access to Naloxone [a drug used to treat an opioid overdose] and support for supervised injection sites.”
Safe-injection sites offer open spaces where those suffering from opioid addictions can safely use the drug without legal repercussions and with the support of medical equipment and services. Although they are not the only solution, they are one of many helpful tools to reduce the growing number of opioid fatalities as research-backed policy moves to counter this health crisis.