In recent years, modern targeted cancer treatments such as chemotherapy, radiation, and surgery have become better at effectively treating the disease. However, these methods continue to be invasive for patients, as they essentially involve racing to kill cancerous cells faster than healthy ones. Fortunately, discoveries in the field of immunotherapy—using the immune system for treatment—are widening the possibilities for successful cancer procedures. This year, the 2018 Nobel Prize for Medicine went to Japanese researcher Tasuku Honjo and American researcher James Allison for their groundbreaking development in immunotherapies, which show promising results in the fight against cancer.
Fundamentally, cancer is a disease of cells. The genes inside a cell control its growth, division, and death. However, sometimes cells ignore these signals and multiply at a facer rate than normal, potentially resulting in cancerous tumours.
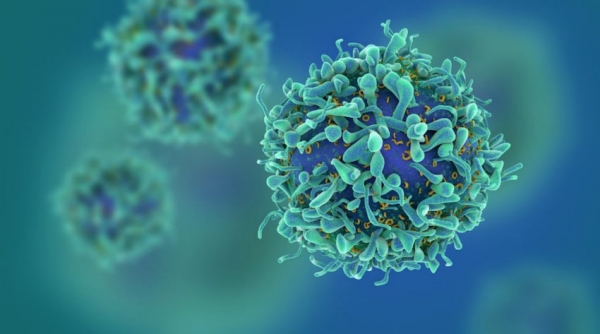
Honjo and Allison’s research largely concerns T-cells, which are white blood cells that play a key role in the immune system by recognizing and destroying abnormal cells, such as the ones that spread cancer. There are a variety of T-cell types including ‘cytotoxic T-cells,’ which kill tumour and virus-infected cells, and ‘helper T-cells,’ which assist other white blood cells in performing their functions.
“Historically, [T-cells] were thought to be CD4 [helper] and CD8 [cytotoxic] in nature, but this simple classification has expanded dramatically in the last decade,” Brian Ward, associate professor in McGill’s Department of Microbiology and Immunology, wrote in an email to The McGill Tribune.
In order to trigger an immune response, all T-cells interact with a complex system of proteins that act as accelerators and brakes. This system is similar to that of a car, which can brake to stop or accelerate to go faster. T-cells can accelerate to destroy cells but also brake before they destroy healthy ones. Deformed cancerous cells spread when the T-cells either are either not acting fast enough or braking before destroying them.
The new research is the result of decades of work. In the 1990s, Allison studied the effects of a protein called CTLA-4, which acts like a brake on T-cells. He was able to develop an antibody to block the protein’s function and, with the brakes cut, T-cells can go on destroying cancer cells beyond what is normally possible.
A few years later, Honjo discovered another brake protein known as PD-1. PD-1 also inhibits T-cells but does so by preventing their activation. Honjo then developed a treatment for cancer based on PD-1 blockage.
Studies have demonstrated the incredible potential of these two novel immunotherapies; many trial patients are experiencing long-term remission and some are even cured. While the anti-PD-1 therapy has been found to be the more effective of the two, combining them has proven to be the most successful option.
“[The] field [of immunotherapy] has already radically changed cancer treatment and will, undoubtedly, change the approach to many autoimmune condition[s] as well as some infectious diseases,” Ward wrote.
In the future, immunotherapy could develop into a cure for many more illnesses than cancer. Its potential is unlimited.